
Cushing syndrome 진단에 대한 호르몬 수치 기준을 정리해 보았습니다. 참고 내용은 최근 개정된 Williams Textbook of Endocrinoloy, 14th edition입니다.
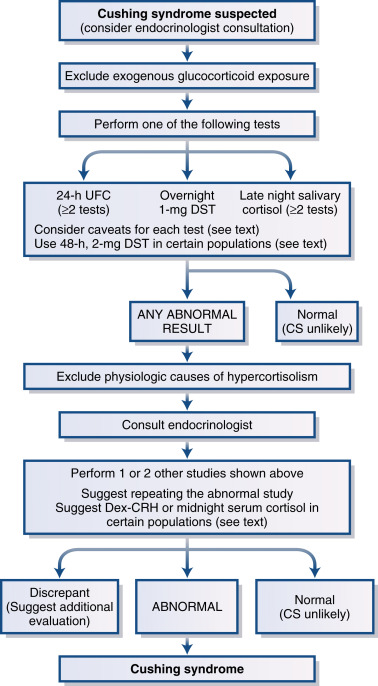
쿠싱 증후군이 의심되는 검사하는 2가지 단계가 있습니다. ① 이 환자가 쿠싱 증후군인가? ② 만일 그렇다면 원인이 무엇인가?
Primary hyperaldosteronism의 경우 PAC. PRA, ARR로 screening test 한 후 양성이면 confirmation test를 진행하는 것처럼 의과대학을 다닐 때는 쿠싱 증후군 screening test와 confirmation test를 구분해서 배웠던 기억이 납니다. 내과 전공의 2년차까지도 그렇게 배웠으나 해리슨 18판이 나오면서 Cushing syndrome의 경우 screening test/confirmation test를 묶었습니다. ① 일단 쿠싱 증후군이 맞는지 확인이 되면 ② 원인 감별을 위한 검사를 진행합니다.
이렇게 쿠싱 증후군이 맞는지 생화학 검사로 확인할 때까지 영상 검사는 시행하지 않는 것이 중요합니다. 쿠싱 증후군에 대한 screening test와 confirmation test는 다음 4가지입니다.
urinary free cortisol
late-night salivary cortisol
overnight dexamethasone
2-mg/48-hour dexamethasone suppression test
쿠싱 증후군이 의심되는 환자에서 4가지 검사 중에 한 가지가 이상이 있는 경우, 다른 나머지 검사들 중 한 가지가 양성이면 쿠싱 증후군 확진입니다. 2가지 검사가 비정상이면 쿠싱 증후군 원인에 대한 검사를 해야 합니다.
Diagnostic criteria that point to Cushing syndrome are a urinary free cortisol (UFC) value greater than the normal range for the assay, a serum cortisol level greater than 1.8 μg/dL (>50 nmol/L) after administration of 1 mg dexamethasone (1-mg DST), and a late-night salivary cortisol concentration greater than 145 ng/dL (>4 nmol/L).
The diagnosis of Cushing’s syndrome: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab . 2008;93:1526–1540.
Screening/confirmation test 기준은?
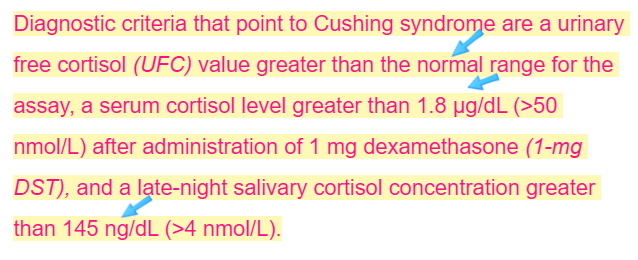
① Urinary free cortisol > 정상 범위
② Late-night salivary cortisol > 145 ng/dL
③ Overnight dexamethasone test > 1.8 μg/dL
④ 2-mg/48-hour dexamethasone suppression test > 1.8 μg/dL
1-mg DST (overnight DST) 기준은 1.8 μg/dL이고 2-mg/48-hour dexamethasone suppression test 기준도 1.8 μg/dL입니다.
|
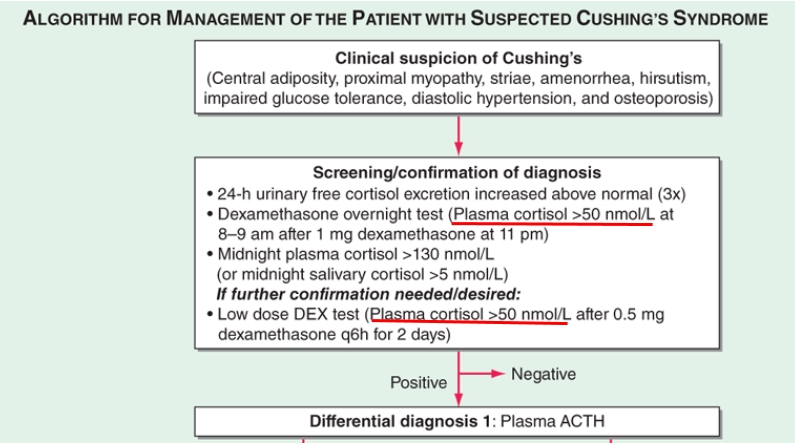
Williams Textbook of Endocrinology, 14th edition In the 48-hour low-dose dexamethasone test, plasma cortisol is measured at 9 am on day 0 and again 48 hours later, after administration of dexamethasone 0.5 mg every 6 hours for 48 hours. Using a postdexamethasone plasma cortisol concentration of less than 50 nmol/L (<1.8 μg/dL) as the cutoff point, this test is reported to have a 97% to 100% true-positive rate and a false-positive rate of less than 1%. UpToDate 2020.09.28 The normal response to the low-dose, two-day test consists of the following: When using specific assays to measure serum cortisol, the recommended criterion for suppression is a serum cortisol <1.8 mcg/dL (<50 nmol/L). Using a serum cortisol concentration <1.8 mcg/dL (50 nmol/L) at 24 or 48 hours as a criterion of normal suppression, one retrospective study correctly identified 98 percent of 245 patients with Cushing's syndrome. |
해리슨 표에 있는 overnight DST, LDST 기준도 plasma cortisol > 50 nmol/L이며 이 값은 1.8 mcg/dL에 해당합니다.
REF. Williams Textbook of Endocrinology, 14th edition
추가기록
해리슨 20판의 Disorders of the Adrenal Cortex를 보면 overnight DST, LDST 기준으로 plasma cortisol > 50 nmol/L (1.8 mcg/dL)이 표에 나와 있습니다.

그러나 Adrenal Gland Disorders에 보면 1-mg overnight dexamethasone test는 <1.8 µg/dL, 0.5 mg dexamethasone every 6 h for 48 h는 <5 µg/dL으로 언급되어 있습니다.
The diagnosis of Cushing’s syndrome requires demonstration of increased cortisol production and abnormal cortisol suppression in response to dexamethasone. For initial screening, measurement of 24-h urinary free cortisol, the 1-mg overnight dexamethasone test (8:00 A.M. plasma cortisol <1.8 µg/dL [50 nmol/L]), or late-night salivary cortisol measurement is appropriate. Repeat testing or performance of more than one screening test may be required. Definitive diagnosis is established in equivocal cases by inadequate suppression of urinary cortisol (<10 µg/d [25 nmol/d]) or plasma cortisol (<5 µg/dL [140 nmol/L]) after 0.5 mg dexamethasone every 6 h for 48 h.
J Clin Endocrinol Metab. 2008;93(5):1526. Epub 2008 Mar 11. [2008 Endocrine Society clinical guidelines]에서는 진단적 코티솔 기준으로 1.8 mcg/dL (50 nmol/L)을 제안합니다. 진단적 기준을 5 µg/dL에서 1.8 mcg/dL로 사용하면 쿠싱 증후군의 민감도는 증가하고 특이도는 감소합니다. Cutoff 값을 점차 올리면 잘못된 비정상 결과들을 줄이지만 쿠싱 증후군 환자를 확인하는 기회를 희생시킵니다.

|
3.4.3 Evidence for the 1-mg DST In normal subjects, the administration of a supraphysiological dose of glucocorticoid results in suppression of ACTH and cortisol secretion. In endogenous Cushing's syndrome of any cause, there is a failure of this suppression when low doses of the synthetic glucocorticoid dexamethasone are given (78). The overnight test is a simple outpatient test. Various doses of dexamethasone have been used, but 1 mg dexamethasone is usually given between 2300 and 2400 h, and cortisol is measured between 0800 and 0900 h the following morning. Higher doses (1.5 or 2 mg) do not significantly improve the accuracy of the test (49). Researchers have used cutoff values for the suppression of serum cortisol from 3.6 to 7.2 μg/dl (100–200 nmol/liter) when measured by modern RIA (79). A widely cited normal response is a serum cortisol less than 5 μg/dl (<140 nmol/liter) (7, 80). Because some patients with Cushing's disease demonstrate suppressibility to dexamethasone, use of this diagnostic criterion misclassified up to 15% of such patients as negative (81, 82). Therefore, to enhance sensitivity, experts have advocated requiring a lower cutoff for suppression of the postdexamethasone serum cortisol to less than 1.8 μg/dl (50 nmol/liter) to achieve sensitivity rates of greater than 95% (83). At the 1.8 μg/dl cutoff, the sensitivity is high with specificity rates of 80%; specificity increases to greater than 95% if the diagnostic threshold is raised to 5 μg/dl (140 nmol/liter) (7). Given our objective of using tests with high sensitivity at this stage, we recommend use of the more stringent cutoff of 1.8 μg/dl. Overall, the evidence in adults indicates that in studies with low prevalence of Cushing's syndrome this test has similar performance as the others recommended for initial testing (2). Although the 1-mg overnight test is used as a screening test for pediatric patients, there are no specific data regarding its interpretation or performance in this population. 3.4.3 Remarks for the 1-mg DST See the earlier comments under 3.4 Remarks for dexamethasone tests. 3.4.4 Evidence for the 48-h, 2 mg/d DST Some endocrinologists prefer to use the 48-h, 2 mg/d low-dose DST (LDDST) as an initial test because of its improved specificity as compared with the 1-mg test. With adequate written instructions for the patient, the LDDST is easily performed in the outpatient setting. As described above (Section 1.0), certain psychiatric conditions (depression, anxiety, obsessive compulsive disorder), morbid obesity, alcoholism, and diabetes mellitus can be characterized by overactivation of the HPA axis but without true Cushing's syndrome, i.e. hypercortisolism is not autonomous. In these conditions, UFC measurements are less useful as an initial test. The optimal test is the LDDST. Previous studies using various doses of dexamethasone and differing criteria for suppression suggest that at least 2 wk of abstinence from alcohol are needed to reduce the false-positive rate (84). First described by Liddle (85) in 1960, the LDDST initially evaluated urinary 17OHCS as an indicator of cortisol suppression. However, using 17OHCS or UFC, sensitivity and specificity rates are less than 70–80%. Use of a serum cortisol end point is simpler and has higher diagnostic accuracy (78). With a cutoff value for suppression of 50 nmol/liter (1.8 μg/dl), the initially reported sensitivity was greater than 95% for adult patients (86). With this approach, the sensitivity for Cushing's syndrome in 36 pediatric patients was 94% (87). With a slightly different protocol and a lower cortisol criterion [38 nmol/liter (1.4 μg/dl)], the sensitivity was 90% in another study (9). Subsequent reports showed lower diagnostic accuracy of the LDDST (7, 88–90). Overall, in 92 patients without Cushing's syndrome, the specificity of the LDDST was 70% (95% confidence interval 69–87%). In 59 patients with Cushing's syndrome, sensitivity was 96% for the LDDST (91). The reasons for this apparent decrease in specificity are unknown. Serum dexamethasone levels were not evaluated; in healthy volunteers, dexamethasone levels 2 h after the last dose were 13.0 ± 6.1 μmol/liter (469.5 ± 220.4 μg/dl) (92). Consequently, the overall evidence in adults indicates that this test has similar or slightly less diagnostic accuracy than the other tests recommended here for initial testing (2). 3.4.4 Remarks for the 48-h, 2 mg/d DST In addition to the general remarks on dexamethasone tests presented in the Initial testing section, there are further considerations for the LDDST. Dexamethasone is given in doses of 0.5 mg for 48 h, beginning at 0900 h on d 1, at 6-h intervals, i.e. at 0900, 1500, 2100, and 0300 h. Serum cortisol is measured at 0900 h, 6 h after the last dose of dexamethasone. Yanovski et al. (9) proposed a different protocol: administering 48 h of dexamethasone at 6-h intervals but beginning at 1200 h and obtaining serum cortisol at 0800 h, exactly 2 h (rather than 6 h as in the usual protocol) after the last dexamethasone dose. For pediatric patients weighing more than 40 kg, the initial adult protocol described above and the adult threshold for normal suppression [<50 nmol/liter (1.8 μg/dl)] are used. For patients weighing less than 40 kg, the dose is adjusted to 30 μg/kg·d (in divided doses) (87). 3.5 Evidence The diagnostic accuracy of various other tests previously advocated for the diagnosis of Cushing's syndrome (urinary 17-ketosteroids, 1600 h or other random cortisol levels, and the insulin tolerance test) is too low to recommend them for testing (49). Other tests, such as the loperamide test, have insufficient evidence for their diagnostic accuracy. The response to those tests used specifically to establish the cause of Cushing's syndrome (e.g. pituitary, adrenal or thoracic imaging, plasma ACTH concentration, CRH stimulation test, 8 mg dexamethasone suppression test) may be both abnormal in healthy people and normal in patients with Cushing's syndrome and therefore are not helpful in establishing the diagnosis (78). 3.6–3.8 Evidence Our recommendations for retesting patients with initially normal test results who develop new or progressive signs or symptoms of Cushing's syndrome comes from the panel's clinical observations and relate to the recognition that the patient's pretest probability of Cushing's syndrome would be higher on retesting and that hypercortisolism may have evolved concomitantly with the progression of the clinical syndrome, enhancing the likelihood that repeat tests would be positive. Similarly, the recommendation to retest patients with suspected cyclic Cushing's syndrome comes from the recognition that these individuals may have normal test results when the disorder is quiescent (93). The performance and interpretation of subsequent testing for Cushing's syndrome requires considerable expertise (both in the clinic and in the laboratory) and may be followed by either complex testing to establish its cause and surgical treatments or expert reassurance of patients that they do not have this condition. Because of this, it is the panel's observation that referral to endocrinology centers with expertise and interest in Cushing's syndrome in patients with abnormal initial testing is likely to be associated with better patient outcomes. The recommendation to perform additional testing in patients with discordant results derives from the knowledge that some patients with Cushing's syndrome, usually those with mild or cyclic disease, may have discordant results. Also, some patients without Cushing's syndrome may have only a minimally abnormal but discordant result. The distinction between these groups is difficult, and there is no one correct diagnostic strategy. The test results' validity should be evaluated in light of the caveats mentioned for specific patient situations and for each test and assay. For example, an abnormal UFC may not be accepted if the specimen volume and creatinine suggest overcollection. Underlying disorders that may cause mild hypercortisolism (Table 2) should be considered and testing repeated when these are treated or resolved. Postponing additional testing to allow progression of clinical and biochemical features may be useful. The patient should be reassured that this poses minimal risk in the setting of mild hypercortisolism |
'내분비내과 > 부신질환' 카테고리의 다른 글
| 쿠싱증후군 치료, 한 쪽 부신이 원인인 경우 (0) | 2021.04.25 |
|---|---|
| 부신기능저하증 환자가 스테로이드를 복용 중 용량 증가를 고려해야 할 상황 (0) | 2021.02.14 |
| [Endocrinology] 부신 우연종, Adrenal incidentalomas (0) | 2020.08.01 |
| [Endocrinology] 선천성 부신증식증 [부신과형성], Congenital adrenal hyperplasia ... nonclassic 21-OHD (0) | 2020.08.01 |
| [Endocrinology] 쿠싱 증후군 진단에서 검사 결과 숫자 암기, 쿠싱 증후군에서 혈장과 침 코티솔의 circadian rhythm 소실 (0) | 2020.08.01 |



