1. 갑상선기능저하증과 고프로락틴혈증
갑상선기능저하증은 고프로락틴 혈증을 유발합니다. 그러나 대부분의 갑상선 기능저하증 환자에서 기저 혈청 프롤락틴 농도는 정상이며, TRH와 같은 자극에 대한 혈청 프롤락틴 반응만 증가합니다. 기저 혈청 프롤락틴 농도가 상승한 몇몇 갑상선 기능저하증 환자에서 갑상선 기능저하증이 교정되면 수치가 정상으로 돌아옵니다. 갑상선 기능저하증을 커진 뇌하수체(thyrotroph hyperplasia, lactotroph hyperplasia, 또는 둘 다 원인으로 인한)와 고프로락틴혈증의 잠재적 원인으로 인식하고 이것을 lactotroph adenoma와 혼동하지 않는 것이 중요합니다. 갑상선 기능저하증에서 고프로락틴혈증의 기전은 알려져 있지 않습니다. TRH의 증가된 시상하부 합성과 TRH에 대한 뇌하수체 반응 증가가 기술되었습니다.
고프로락틴혈증이 유일하게 갑상선기능저하증의 결과라면, 갑상선기능저하증이 교정이 되면 고프로락틴혈증은 없어질 것이며 다른 치료는 필요하지 않습니다.
TRH stimulates PRL secretion. Estrogen stimulates PRL gene transcription and secretion, explaining why women have higher PRL levels, particularly during the periovulatory menstrual phase.
Up to 20% of patients with hypothyroidism have elevated PRL levels. Treatment of hypothyroidism with thyroid hormone normalizes serum PRL if the hyperprolactinemia is due to thyroid hormone deprivation.
Primary hypothyroidism can cause hyperprolactinemia and galactorrhea, because increased levels of thyroid-releasing hormone increase secretion of prolactin as well as thyroid-stimulating hormone (TSH).
Primary hypothyroidism is easily ruled out by absence of elevated TSH.
The hyperprolactinemia of hypothyroidism is related to several mechanisms. In response to the hypothyroid state, a compensatory increase in the discharge of central hypothalamic thyrotropin-releasing hormone results in increased stimulation of prolactin secretion. Furthermore, prolactin elimination from the systemic circulation is reduced, which contributes to increased prolactin concentrations. Primary hypothyroidism can be associated with diffuse pituitary enlargement, which will reverse with appropriate thyroid hormone replacement therapy.
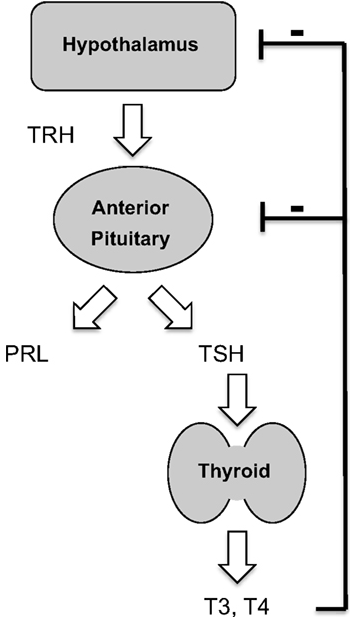
TRH is a hypothalamic tripeptide that sits atop the hypothalamic/pituitary/thyroid axis; its primary function is stimulating release of thyrotropin (TSH) from the anterior pituitary gland. However it can also cause an increase in prolactin (PRL) secretion!
2. Postmenopausal women에서 hyperprolactinemia

Hyperprolactinemia causes typical symptoms in premenopausal women and in men, but not in postmenopausal women.
Postmenopausal women — Postmenopausal women, by definition, are already hypogonadal, and hyperprolactinemia does not change that situation. Because postmenopausal women are also markedly hypoestrogenemic, galactorrhea is rare. Hyperprolactinemia in these women is recognized only in the relatively unusual situation when a lactotroph adenoma becomes so large as to cause headaches or impair vision or is detected as an incidental finding when a magnetic resonance imaging (MRI) study is performed for an unrelated reason.

In adult premenopausal females, the typical presentation is galactorrhea and oligomenorrhea. Because galactorrhea is enabled by estrogen, postmenopausal women, who are generally deficient in estrogen, do not develop galactorrhea despite elevated prolactin levels.

Hyperprolactinemia is not a common finding in postmenopausal women. Prolactinomas detected after menopause are usually macroadenomas. Due to atypical clinical features they may remain unrecognized for a long period of time. Interestingly the growth potential of prolactinomas remains after menopause. Most tumors are invasive and present with high prolactin levels.






Prolactinomas diagnosed during the post-menopausal period are rare. Tumor induced menstrual disturbances that lead to the diagnosis in young patients cannot be detected in women already amenorrheic as a function of menopause. Tumors may remain unrecognized; therefore the true prevalence of prolactinomas during the menopausal period cannot be accurately determined.

In postmenopausal women, prolactinomas are rarely encountered and usually do not present with hyperprolactinemia-related symptoms as these are dependent mostly on intact ovarian function. As this particular type of prolactinoma is probably underdiagnosed and not reported enough in the endocrine literature, we have summarized our experience with these women.
Prolactinomas are more common in young and fertile females, 20–40 years-old, while they are rarely diagnosed in pre-pubertal girls and postmenopausal women.
If the tumor develops during this period, it usually stays silent if not diagnosed incidentally, or presents only after years of insidious tumor growth, when the tumor becomes large enough and invasive to develop symptoms of a pituitary mass. Therefore, the true incidence of PRL-secreting adenomas in postmenopausal woman is unknown.

--------------------------------------------------------------------
It is worth noting that many premenopausal women with hyperprolactinemia do not have galactorrhea, and many with galactorrhea do not have hyperprolactinemia.This is because galactorrhea requires adequate estrogenic or progesterone priming of breast.Conversely, isolated galactorrhea with normal prolactin levels occurs due to increased sensitivity of the breast to the lactotrophic stimulus. Thus, galactorrhea is very uncommon in postmenopausal women.
rolactinomas are divided into two groups: (1) microadenomas (smaller than 10 mm) which are more common in premenopausal women, and (2) macroadenomas (10 mm or larger) which are more common in men and postmenopausal women.

대표사진 삭제
사진 설명을 입력하세요.



