헬리코박터 파일로리 치료는 전형적으로 항생제와 PPI 병합입니다. 치료 regimen을 정하는데 도움이 되도록 환자에게 이전 항생제 노출력에 대해 물어야 합니다. 헬리코박터 파일로리 감염에 대해 100% 치료율을 보이는 regimen은 없습니다. 선호되는 강도를 표현하기 위해 recommend와 suggest 표현을 사용하였습니다.
H. pylori is typically treated with a combination of antibiotics plus a proton pump inhibitor (PPI). Patients should be asked about previous antibiotic exposure to help guide the treatment regimen. There is no regimen with a 100% cure rate for H. pylori infection, and there are few, if any, regimens with a 90% cure rate. The authors used the terms recommended and suggested to express their preferences.
RECOMMENDED
Clarithromycin triple therapy는 PPI, clarithromycin, amoxicillin/또는 metronidazole 14일 요법입니다. Clarithromycin에 대한 헬리코박터 파일로리 내성 효과는 잘 입증되어 있습니다. Clarithromycin에 대한 내성이 15%보다 큰 지역과 이전에 macrolide 노출력이 있는 환자에서는 clarithromycin은 피해야 합니다.
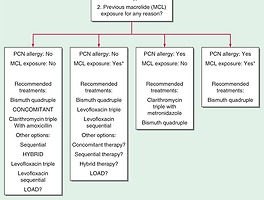
Clarithromycin triple therapy consists of a PPI, clarithromycin(Biaxin), and amoxicillin or metronidazole (Flagyl) for 14 days. The effect of H. pylori resistance to clarithromycin is well documented. Clarithromycin should be avoided in locations where resistance is greater than 15% and in patients with any previous macrolide exposure.
Bismuth quadruple therapy는 PPI, bismuth, tetracycline, nitroimidazole 10-14일 요법입니다. 이것은 특히 macrolide 노출력이 있는 환자 또는 페니실린 알레르기 환자에서 좋은 선택일 수 있습니다. 비록 metronidazole 내성이 이 regimen의 효과에 영향을 줄지라도 clarithromycin triple therapy만큼 현저하지 않습니다. Bismuth quadruple therapy는 clarithromycin 내성이 높거나 이전 macrolide 노출력이 있는 환자에서 1차 치료로 강하게 고려되어야 합니다.
Bismuth quadruple therapy consists of a PPI, bismuth, tetracycline, and a nitroimidazole for 10 to 14 days. It may be a particularly good option in patients with macrolide exposure or who are allergic to penicillin. Although metronidazole resistance impacts the effectiveness of this regimen, it is not nearly as profound as with clarithromycin triple therapy. Bismuth quadruple therapy should be strongly considered as first-line treatment where clarithromycin resistance is high or in patients with any previous macrolide exposure.
Concomitant therapy는 PPI, clarithromycin, amoxicillin, nitroimidazole(tinidazole 또는 metronidazole) 10-14일 요법입니다.
Concomitant therapy consists of a PPI, clarithromycin, amoxicillin, and a nitroimidazole (tinidazole [Tindamax] or metronidazole) for 10 to 14 days. This regimen is a promising option that has been shown in international studies to be at least as effective as clarithromycin triple therapy with similar tolerability. Limited data show that the effects of clarithromycin resistance with this regimen are less than with clarithromycin triple therapy. A duration of 10 to 14 days seems appropriate, although studies
to assess whether extending therapy to 14 days improves eradication are ongoing.
SUGGESTED
Sequential therapy consists of a PPI and amoxicillin for five to seven days followed by a PPI, clarithromycin, and a nitroimidazole for five to seven days. Although 10 days of sequential therapy appears to be a viable alternative to 14 days of clarithromycin triple therapy, 10 days of sequential therapy has not been shown to be superior to 14 days of clarithromycin triple therapy. Extending sequential therapy to 14 days may improve eradication rates, but more studies are needed. The complexity of sequential therapy may limit its use.
Hybrid therapy, a cross between sequential and concomitant therapies, consists of a PPI and amoxicillin for seven days followed by a PPI, amoxicillin, clarithromycin, and a nitroimidazole for seven days. This regimen is a promising option that has been shown in international studies to be at least as effective as clarithromycin triple therapy with similar tolerability. Although randomized controlled trials
showed hybrid therapy to be similar to concomitant therapy, the complexity of hybrid therapy may limit its use.
Levofloxacin triple therapy consists of a PPI, levofloxacin(Levaquin), and amoxicillin for 10 to 14 days. Levofloxacin is a fluoroquinolone with in vitro antimicrobial activity against gram-positive and gram-negative bacteria, including H. pylori. The few data that exist suggest that fluoroquinolone resistance may be as high, if not higher, than clarithromycin resistance in North America. There is also a lack of data regarding the impact of fluoroquinolone resistance on treatment. Levofloxacin triple therapy for 10 to 14 days appears to be a comparable alternative to clarithromycin triple therapy. The best options appear to be fluoroquinolone-containing sequential therapy (a PPI and amoxicillin for five to seven days followed by a PPI, a fluoroquinolone, and nitroimidazole for five to seven days) or LOAD therapy (levofloxacin, omeprazole [Prilosec], nitazoxanide [Alinia], and doxycycline for seven to 10 days).
1. Am Fam Physician. 2018 Jan 15;97(2):135-137.
2. Am J Gastroenterol 2017; 112:212–238; doi: 10.1038/ajg.2016.563 ; published online 10 January 2017
'소화기내과(위장관) > 소화성궤양' 카테고리의 다른 글
| H. pylori 항생제 내성과 검사, 2017 ACG clinical guideline (0) | 2018.09.16 |
|---|---|
| H. pylori 감염을 치료할 때 성공적인 제균을 예견하는 요인은 무엇입니까? 2017 ACG clinical guideline (0) | 2018.08.30 |
| 진통소염제 관련 위점막 손상에 대한 치료, 예방에 대한 내용 Harrison's 20th edition (0) | 2018.08.18 |
| H. pylori infection 환자에서 항생제 선택 (0) | 2018.08.18 |
| 헬리코박터 파일로러 검사와 치료의 적응증, 2017 ACG clinical guideline (0) | 2018.08.16 |