1. 임신 중 TSH가 2.5 mU/L보다 적은 경우 [이전과 내용이 다름]
https://blog.naver.com/sjloveu2/221579210583
2. 임신 중 TSH >4 mU/L 인 경우 [이전과 내용이 같음]
https://blog.naver.com/sjloveu2/221467364287
3. 임신 중 TSH 2.6 - 4 mU/L인 경우 [이전과 내용이 다름]
For pregnant women with TSH in this range, we individualize the decision to treat based upon patient characteristics, values, and preferences. Some experts, including one editor of this topic, do not treat euthyroid pregnant women. Other experts, including the author and another editor of this topic, offer treatment to selected pregnant women based on the presence or absence of TPO antibodies, which have been associated with adverse pregnancy outcomes (eg, early pregnancy loss)
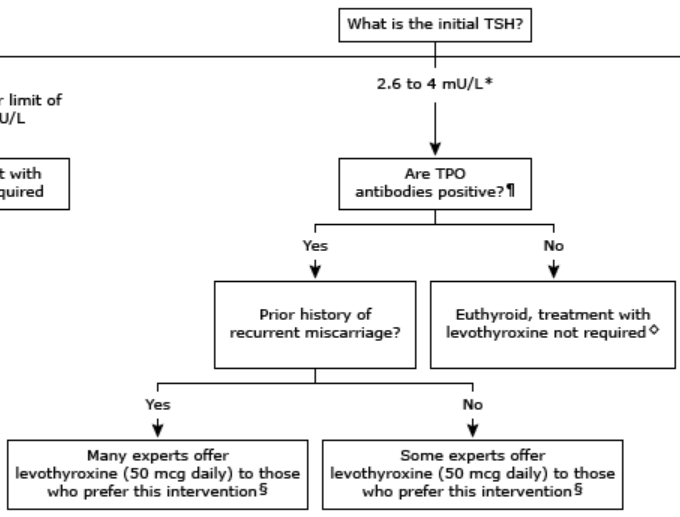
•TPO antibodies positive
For pregnant women with a TSH between 2.6 mU/L and the upper limit of the trimester-specific reference range (or 4.0 mU/L if trimester-specific range unavailable), positive TPO antibodies, and a history of recurrent miscarriage, many experts (including the author and one editor of this topic) offer treatment with T4 (50 mcg daily) to those who prefer this intervention. This is based on weak evidence in view of conflicting data regarding the efficacy of T4 for reducing the risk of miscarriage. However, carefully monitored thyroid hormone treatment is safe.
In the absence of a history of recurrent miscarriage, some experts (including one editor of this topic) also offer T4 (50 mcg daily) to those who prefer this intervention (based on weak evidence).
If a decision is made not to treat, TSH should be reassessed every four weeks during the first trimester and once each in the second and third trimester to monitor for the development of hypothyroidism. If TSH rises above the population and trimester-specific upper limit of normal (approximately 4 mU/L), we begin treatment with T4.
•TPO antibodies negative
For pregnant women with a TSH between 2.6 mU/L and the upper limit of the trimester-specific reference range (or 4.0 mU/L if trimester-specific range unavailable), and negative TPO antibodies, we do not treat with T4.
For women at high risk for developing hypothyroidism (eg, history of radioiodine treatment, hemithyroidectomy, or exposure to high-dose irradiation of the head and neck), we monitor for the development of hypothyroidism by reassessing TSH approximately every four weeks during the first trimester and once during each of the second and third trimesters. If TSH rises above the population and trimester-specific upper limit of normal (approximately 4 mU/L), we begin treatment with T4.
REF. UpToDate 2019.07.07
'내분비내과 > 갑상선기능저하증' 카테고리의 다른 글
| 갑상선기능저하증에서 빈혈, Anemia in hypothyroidism (0) | 2020.03.07 |
|---|---|
| 임신부에서 갑상선 기능 저하증으로 약물 복용 중 추적 검사와 용량 조정 (0) | 2019.08.29 |
| 임신 중 TSH가 2.5 mU/L보다 적은 경우 (0) | 2019.07.06 |
| 임신 중 갑상선 기능저하증 [정리], Hypothyroidism in pregnancy (1) | 2019.03.22 |
| 임신부 갑상선 기능저하증 ③ Trimester-specific LLM < TSH < 2.5mU/L (0) | 2019.03.06 |



