http://www.pathologyoutlines.com/topic/stomachlymphocyticgastritis.html














Stomach
Gastritis
Lymphocytic gastritis
Author: Matthew Morrow, M.D.
Senior Author: Raul S. Gonzalez, M.D.
Editor-in-Chief: Debra Zynger, M.D.
Topic Completed: 7 May 2019
Revised: 7 May 2019
Copyright: 2003-2019, PathologyOutlines.com, Inc.
PubMed Search: lymphocytic gastritis[title]
Definition / general
A pattern of gastric mucosal injury characterized by increased intraepithelial lymphocytes (> 25 per 100 epithelial cells) and increased chronic inflammatory cells in the lamina propria
Essential features
Associated with Helicobacter pylori infection and celiac disease, among other etiologies
Variable clinical presentation
Uncertain pathogenesis
Terminology
The older entity “varioliform gastritis” (endoscopic mucosal appearance of small nodules with central erosions and enlarged rugal folds) appears to represent a subset of lymphocytic gastritis (J Pathol 1989;158:19)
ICD coding
ICD-10: K52.89 - other specified noninfective gastroenteritis and colitis
Epidemiology
Rare, with a prevalence of < 0.3% in gastric biopsies (Odze and Goldblum: Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas, 3rd Edition, 2015)
Presents around the sixth decade of life (Am J Surg Pathol 1999;23:153)
No sex predilection
Common etiologic associations include celiac disease (Am J Surg Pathol 1999;23:153)
Also associated with HIV infection, Crohn disease, Ménétrier disease, NSAIDs and lymphocytic or collagenous colitis
Unknown etiology in up to 20% of cases (Am J Surg Pathol 1999;23:153)
Rare in children but seen predominately with celiac disease; may suggest a more severe disease course in this setting (Pediatr Dev Pathol 2011;14:280)
Sites
Antral predominance or diffuse involvement may be associated with celiac disease (J Clin Pathol 1999;52:815)
Corpus predominance may be associated with H. pylori infection (Am J Surg Pathol 1999;23:153)
Pathophysiology
Uncertain pathogenesis overall
Due to its association with celiac disease and H. pylori, it has been proposed to be a local immune response to luminal antigens such as gliadin and Helicobacter antigens (Am J Surg Pathol 1999;23:153)
Clinical features
Dyspepsia, abdominal pain and iron deficiency anemia have been reported but presenting symptoms are variable (Pathol Case Rev 2008;13:167)
Predominately recurrent vomiting, epigastric pain or chronic diarrhea is seen in pediatric patients (J Pediatr 1994;124:57)
Cases associated with endoscopic varioliform gastritis may present with weight loss and anorexia (Gut 1990;31:282)
Cases associated with Ménétrier disease may present with protein losing enteropathy (Hum Pathol 1991;22:379)
Diagnosis
Established by gastric biopsy
Case reports
2 year old child autopsy findings after presenting with hepatic failure (Ann Diagn Paed Pathol 1998;2:27)
47 year old woman and 57 year old man with H. pylori and associated gastric MALT lymphoma (Korean J Gastroenterol 2005;45:354)
63 year old man with gastric adenocarcinoma and total gastrectomy (Gut 1991;32:1565)
77 year old man with worsening anemia (Gastrointest Endosc 2001;54:251)
84 year old man with abdominal pain and varioliform gastritis seen on EGD (Ann Gastroenterol 2018;31:520)
Treatment
Targets the underlying associated etiology
Can spontaneously regress (Aliment Pharmacol Ther 2006;23:473)
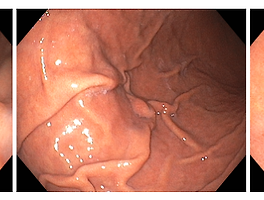
Clinical images
Images hosted on other servers:

Varioliform gastritis:
multiple nodules with
central mucosal
atrophy / erosion
Gross description
Small nodules with central erosions and enlarged rugal folds (“varioliform gastritis”)
Early studies suggested this finding in 80% of cases
Subsequent articles reported incidence of 4% to 30% (Pathol Case Rev 2008;13:167)
Additional findings: small elevated plaques, superficial erosions, nodular appearance, thickened folds
Unremarkable appearance in up to 50% of cases (J Clin Pathol 1995;48:939, Gut 1988;29:1258)
Hypertrophic gastric folds has been described in cases of Ménétrier disease (Hum Pathol 1991;22:379)
Microscopic (histologic) description
Defined by increased gastric intraepithelial lymphocytes (> 25 per 100 epithelial cells)
Intraepithelial lymphocytosis is typically greater in the surface epithelium
Most cases show around 35 - 75 surface intraepithelial lymphocytes per 100 epithelial cells (Gut 1990;31:282)
Lymphoplasmacytic expansion of the lamina propria can be additionally seen
Intraepithelial neutrophils may be seen, especially in the setting of H. pylori infection or mucosal erosion
Lymphoepithelial lesions are not present
Microscopic (histologic) images
Contributed by Matthew Morrow, M.D.

Increased intraepithelial lymphocytes




Increased intraepithelial lymphocytes, expanded lamina propria

Biopsy from area of nodular gastric mucosa
Positive stains
Lymphocytes are predominately CD3 positive T cells with CD8 co-expression
Sample pathology report
Stomach, biopsy:
Corpus and antral mucosa with chronic inactive gastritis with increased intraepithelial lymphocytes (see comment)
Immunostain for Helicobacter species is negative
Comment: The finding of intraepithelial lymphocytosis is consistent with lymphocytic gastritis, which may be associated with celiac disease, H. pylorigastritis, viral infection, Crohn disease, certain medications and other etiologies
Differential diagnosis
Often causes a mass lesion, unlike lymphocytic gastritis
Patchy increased intraepithelial lymphocytes can be seen in MALT lymphoma (Korean J Pathol 2007;41:289)
Lymphocytes in MALT lymphoma are CD20+ B cells
Lymphoma may display an infiltrative pattern with lymphoepithelial lesions and architectural distortion
Cytologic atypia may be present
Curved slender bacteria present in the superficial mucus layer and along the surface of gastric epithelial cells
Neutrophils and germinal centers may be seen
Chronic gastritis, such as mononuclear expansion of the lamina propria seen in lymphocytic gastritis, should prompt scrutiny for Helicobacter organisms
Helicobacter immunostain, Giemsa and silver stains highlight organisms
Additional references
Board review question #1

The image above is from an antral biopsy from a 9 year old boy. What additional histological finding is most likely to be present in this patient?
A. Increased intraepithelial eosinophils with eosinophilic microabscesses in the upper esophagus
B. Curved bacteria rods present in the superficial mucus layer of the stomach
C. Duodenal increased intraepithelial lymphocytes, crypt hyperplasia and villous blunting
D. Duodenal villous blunting, crypt hyperplasia and focal surface epithelial “tufting”
Board review answer #1
C. Lymphocytic gastritis is most commonly seen in a background of celiac disease in children (intraepithelial lymphocytes, crypt hyperplasia and villous blunting in the duodenum) and may portend a more severe disease course. Helicobacter infection (choice B) would be more likely in an adult patient.
Board review question #2
Aside from increased intraepithelial lymphocytes, what other histologic feature in the stomach is commonly described in lymphocytic gastritis?
A. Lymphoepithelial lesions
B. Lymphoplasmacytic expansion of the lamina propria
C. Loss of parietal cells
D. Increased subepithelial collagen deposition
Board review answer #2
B. Lymphoplasmacytic expansion of the lamina propria is also commonly seen in lymphocytic gastritis.
'소화기내과(위장관) > 위내시경' 카테고리의 다른 글
| 2020 내시경 세부전문의 갱신, 회복 (0) | 2020.04.20 |
|---|---|
| CLOtest 색변화 (1) | 2019.10.19 |
| 위내시경, 주름 펴기 (0) | 2018.09.22 |
| 글리코겐 가시세포종, 식도, Glycogenic acanthosis (0) | 2018.09.22 |
| 위 용종, 위저선 용종, Gastric polyps, fundic gland polyps (0) | 2018.04.19 |