헬리코박터 파일로리 제균에 대한 해리슨 20판 내용

1. In vitro에서 헬리코박터 균에 많은 항생제들이 감수성이 있을지라도 보통 단일 항생제는 성공적이지 못합니다.
2. 현행 regimen는 PPI와 2개 또는 3개의 항생제를 병합하여 10-14일 동안 사용합니다.
Although H. pylori is susceptible to a wide range of antibiotics in vitro, monotherapy is not usually successful, probably because of inadequate active antibiotic delivery to the colonization niche. Clinical failure of monotherapy prompted the development of multidrug regimens. Current regimens consist of a PPI and two or three antimicrobial agents given for 10–14 days. The optimal regimens vary in different parts of the world, depending on the known rates of primary antibiotic resistance in most H. pylori strains in a particular locale. For this reason, guidelines on optimal regimens for H. pylori eradication in individual countries are evolving, and physicians should refer to the most up-to-date local guideline.
1. 헬리코박터 파일로리 치료에서 가장 중요한 치료 성공 요인은 1) 환자의 약제 복용 순응도와 2) 내성이 없는 약제의 사용입니다.
2. 작은 실수(깜박 잊고 복용하지 않음)에도 치료 실패는 일반적이고 종종 내성을 갖게 합니다.
3. 전 세계적으로 1차 클래리스로마이신 내성률이 충분히 높아서 클래리스로마이신과 다른 하나의 항생제를 포함한 요법은 종종 실패합니다. 클래리스로마이신과 다른 2개이 항생제를 포함한 요법은 비록 클래리스로마이신에 대한 내성이 있을지라도 헬리코박터 파일로리 제균 가능성이 있으므로 치료 선택(option)으로 남아 있습니다.
4. 비록 시간 간격이 멀지라도 클래리스로마이신이나 플루오로퀴놀론에 노출되었다면, 이 항생제들을 보통 피해야 합니다. 아목시실린이나 테트라사이클린 내성은 비록 이전에 투여되었을지라도 일반적이지 않습니다. 메트로니다졸 내성은 단지 부분적입니다. 따라서 이와 같은 항생제를 이전에 투약받았을지라도 피해야 힐 이유는 없습니다.
The two most important factors in successful H. pylori treatment are the patient’s close compliance with the regimen and the use of drugs to which the patient’s strain of H. pylori has not acquired resistance. Treatment failure following minor lapses in compliance is common and often leads to acquired resistance. To stress the importance of compliance, written instructions should be given to the patient, and minor side effects of the regimen should be explained. Increasing levels of primary H. pylori resistance to clarithromycin, levofloxacin, and—to a lesser extent—metronidazole are of growing concern. In most parts of the world (the main exception being northwestern Europe), the rate of primary clarithromycin resistance is sufficiently high that regimens containing clarithromycin plus one other antibiotic often fail; regimens with clarithromycin and two other antibiotics remain an option as the other two antibiotics are likely to eradicate H. pylori even if the strain is clarithromycin resistant. When a patient is known to have been exposed—even distantly—to clarithromycin or a fluoroquinolone, these antibiotics usually should be avoided. Resistance to amoxicillin or tetracycline is unusual, even if these antibiotics have been given previously, and resistance to metronidazole is only partial; thus there is no need to avoid using these antibiotics whether or not they have been previously prescribed. Assessment of antibiotic susceptibilities before treatment would be optimal but is not usually undertaken because endoscopy and mucosal biopsy are necessary to obtain H. pylori for culture and because most microbiology laboratories are inexperienced in H. pylori culture. If initial H. pylori treatment fails, the usual approach is empirical re-treatment with another drug regimen(TABLE 158-2). The third-line approach ideally should be endoscopy, biopsy, and culture plus treatment based on documented antibiotic sensitivities. However, empirical third-line therapies are often used.
Non-pylori gastric helicobacters are treated in the same way as H. pylori. However, in the absence of trials, it is unclear whether a positive outcome always represents successful treatment or whether it is sometimes due to natural clearance of the bacteria.
TABLE 158-2 Commonly Recommended Treatment Regimens for Helicobacter pylori
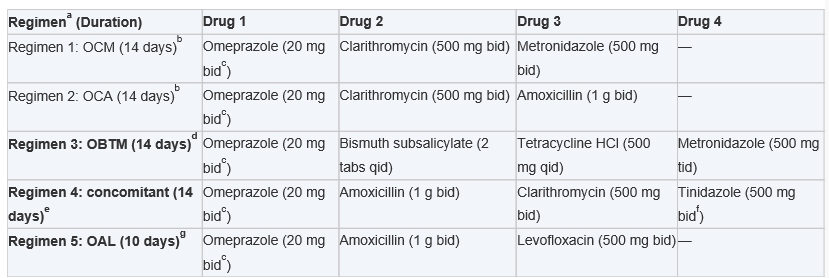
aThe recommended first-line regimens for most of the world are shown in bold type.
bThis regimen should be used only for populations in which the prevalence of clarithromycin-resistant strains is known to be <20%. In practice, this restriction limits the regimens’ appropriate range mainly to northern Europe.
cMany authorities and some guidelines recommend doubling this dose of omeprazole, as trials show resultant increased efficacy with some antibiotic combinations. Omeprazole may be replaced with any proton pump inhibitor at an equivalent dosage. Because extensive metabolizers of PPIs are prevalent among Caucasian populations, many authorities recommend esomeprazole (40 mg bid) or rabeprazole (20 mg bid), particularly for regimens 4 and 5.
dData supporting this regimen come mainly from Europe and are based on the use of bismuth subcitrate (1 tablet qid) and metronidazole (400 mg tid). This is a recommended first-line regimen in most countries and is the recommended second-line regimen in northern Europe.
eThis regimen may be used as an alternative to regimen 3.
fMetronidazole (500 mg bid) may be used as an alternative.
gThis regimen is used as second-line treatment in many countries (particularly where quadruple or concomitant therapy is used as the first-line regimen) and as third-line treatment in others. It may be less effective where rates of fluoroquinolone use are high and is more likely to be ineffective if there is a personal history of fluoroquinolone use for previous treatment of other infections.
REF. Harrison's 20th edition


