
임신 20주 이전에 ㉠ 병력에 근거하여 또는 ㉡ 적어도 4시간 간격으로 2회 측정한 혈압이 수축기 140 이상 또는 이완기 90 이상인 중증이 아닌 만성 고혈압 임신부에서 고혈압 치료를 권고합니다.
- 전통적으로 혈압이 160/110 이상인 중증 만성 고혈압인 경우에만 임신부에서 치료를 해 왔음. 그 이유는 fetal safty 관점과 임신부에게 이득이 된다는 증거 부족 때문이었음. * 160/100 mmHg 이하 혈압을 mild chronic hypertension.
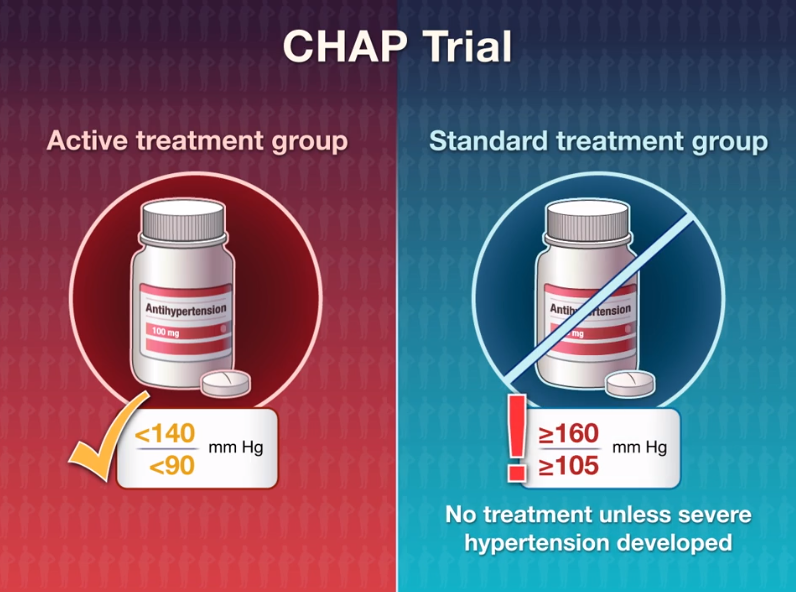
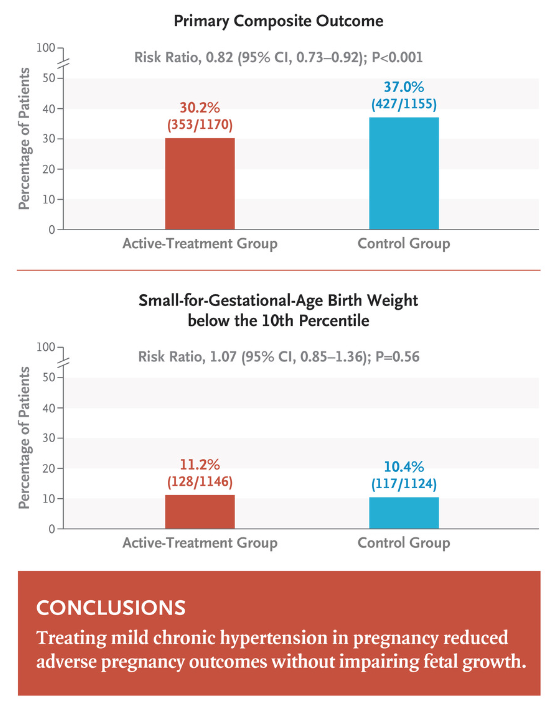
- Chronic Hypertension and Pregnancy (CHAP) trial에서 2400명의 23주 미만 임신부를 대상으로 <140/90 이하로 유지하기 위한 적극적 치료 그룹과 160/105 이상인 경우에만 치료를 하는 보통 그룹 (대조군)으로 무작위 할당. 적극적 치료 그룹에서 의학적으로 필요했던 <35주 조산 (12.2% 대 16.7%), 전자간증 (23.3% 대 29.1%)을 포함한 composite adverse pregnancy outcome의 18% 상대적 감소.
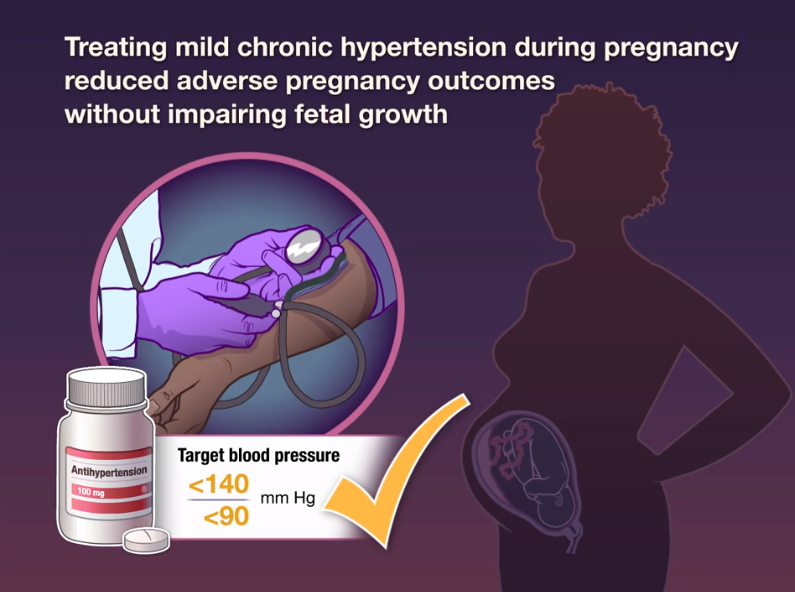
- 결론은 mild chronic hypertension인 임신부에서 혈압이 160/100 이상인 경우메만 치료하는 것보다 140/90를 목표 혈압으로 치료하는 것이 small-for-gestational-age birth weight 증가 없이 더 나은 임신 결과와 관련이 있었음.
BACKGROUND
The benefits and safety of the treatment of mild chronic hypertension (blood pressure, <160/100 mm Hg) during pregnancy are uncertain. Data are needed on whether a strategy of targeting a blood pressure of less than 140/90 mm Hg reduces the incidence of adverse pregnancy outcomes without compromising fetal growth.
METHODS
In this open-label, multicenter, randomized trial, we assigned pregnant women with mild chronic hypertension and singleton fetuses at a gestational age of less than 23 weeks to receive antihypertensive medications recommended for use in pregnancy (active-treatment group) or to receive no such treatment unless severe hypertension (systolic pressure, ≥160 mm Hg; or diastolic pressure, ≥105 mm Hg) developed (control group). The primary outcome was a composite of preeclampsia with severe features, medically indicated preterm birth at less than 35 weeks’ gestation, placental abruption, or fetal or neonatal death. The safety outcome was small-for-gestational-age birth weight below the 10th percentile for gestational age. Secondary outcomes included composites of serious neonatal or maternal complications, preeclampsia, and preterm birth.
RESULTS
A total of 2408 women were enrolled in the trial. The incidence of a primary-outcome event was lower in the active-treatment group than in the control group (30.2% vs. 37.0%), for an adjusted risk ratio of 0.82 (95% confidence interval [CI], 0.74 to 0.92; P<0.001). The percentage of small-for-gestational-age birth weights below the 10th percentile was 11.2% in the active-treatment group and 10.4% in the control group (adjusted risk ratio, 1.04; 95% CI, 0.82 to 1.31; P=0.76). The incidence of serious maternal complications was 2.1% and 2.8%, respectively (risk ratio, 0.75; 95% CI, 0.45 to 1.26), and the incidence of severe neonatal complications was 2.0% and 2.6% (risk ratio, 0.77; 95% CI, 0.45 to 1.30). The incidence of any preeclampsia in the two groups was 24.4% and 31.1%, respectively (risk ratio, 0.79; 95% CI, 0.69 to 0.89), and the incidence of preterm birth was 27.5% and 31.4% (risk ratio, 0.87; 95% CI, 0.77 to 0.99).
CONCLUSIONS
In pregnant women with mild chronic hypertension, a strategy of targeting a blood pressure of less than 140/90 mm Hg was associated with better pregnancy outcomes than a strategy of reserving treatment only for severe hypertension, with no increase in the risk of small-for-gestational-age birth weight. (Funded by the National Heart, Lung, and Blood Institute; CHAP ClinicalTrials.gov number, NCT02299414. opens in new tab.)
REF. N Engl J Med 2022; 386:1781-1792
UpToDate 2022.07.30
'심장내과 > 고혈압' 카테고리의 다른 글
| 텔미트렌정, 텔미누보정, 텔미트렌에스정, 텔미로젯정, 누보로젯정 [종근당] (0) | 2023.01.03 |
|---|---|
| 로제텔핀정 (Rosuvastatin + Ezetimibe + Telmisartan + Amlodipine) (0) | 2022.11.09 |
| 이달비정, 아질사르탄메독소밀칼륨 [Edarbi Tab.] (0) | 2022.06.26 |
| 이완기 단독 고혈압, 수축기 혈압이 정상일 때 약물 치료 여부 (0) | 2022.06.11 |
| 듀카브 플러스 [듀카브 + 하이드로클로로티아지드] (0) | 2022.06.01 |



